Let’s Make Informed Decisions Around School Reopening
Paul Minshull, CEO and Founder, Covid-19 Solution Architect
Contributions by: Arsa Nikzad, Data Science Lead and Marija-Zivkovic-Gojovic, Phd with published paper on pandemic modeling
We believe this report provides insight on how a rigorous forecasting approach can inform better decisions, on the subject of school reopening. We believe that Canada and Ontario, need to evolve their approach to Covid-19 to more localized decision making which starts with forecasting each region. One size does not fit all. That was ok when the country was in pandemic reactive mode in wave I, but we should have taken advantage of June-Aug to become proactive.
Aside from the forecasts, aligning parties to a common goal is critical. 20 years of working with successful global companies have taught us that. The misalignment of key stakeholders here in Ontario (Ministry of Health, teacher’s unions, local public health teams, school boards) does not instill the confidence we should all feel as kids return to school.
Scarsin conducted this analysis independently, no funding from any party for this analysis. Our objective is to leverage our global expertise, Covid-19 platform and significant research on this topic to provide evidence based answers to key questions for Canadians.
Call to Action
Scarsin has been trying since May to engage healthcare decision makers to introduce our solution at the Federal (PHAC, Health Canada), and Ontario (Premier’s office, Management of Emergency Operations center [MEOC]…) level. Unfortunately, we have not had the opportunity to demonstrate our solution to any of them. We remain open to doing so. We are in a pandemic, shaking the foundation of our country, the best technologies should be fighting this together. The Scarsin forecasting platform has over 15 years’ experience helping with multibillion-dollar proactive decisions in the private sector. We believe our decision support system can help!
Scarsin has invested thousands of hours in this Covid-19 solution since March 13 based on Canada and Ontario’s call to action for innovative solutions. We have a team of experts including experience in pandemic modeling. We are working with a large Ontario health region (not HR1 or HR2 referred to in the analysis). They are innovators and saw the opportunity quickly once they saw an early demonstration in May.
We invite other health regions / school boards to reach out to info@scarsin.com (I personally review this inbox) to discuss the solution and see a demonstration of your region. Get proactive!

Key Questions for Exploration
This analysis will provide insights on School Reopening questions:
- Is the risk to opening schools at the same time equal across health regions/boards?
- Can opening schools accelerate the spread of Covid-19 in health regions/boards?
- How much of an impact do the strategies below have on reducing transmission in school?
- Use of masks in younger children 4-9 yrs
- Avoidance strategies (limiting the interactions with schools – alternating days for high school, opting out to online…)
- Other non-pharmaceutical interventions (NPIs) such as social distancing, cleaning, ventilation
- What would be the impact of an intermittent school closure policy on transmission?
- How important is “deep scenario forecasting” to making good decisions for schools?
The Scarsin Covid-19 decision support system measures a wide range of key metrics across various compartments. See model flow on page 9. We are going to focus mostly on Reported case metrics as this the measure most people are familiar with. It is however important to note that Reported cases represent a minority of the actual Covid-19 infections based on levels of testing, asymptomatic cases and mild symptomatic cases. The most important metrics in terms of the healthcare system are the number/severity of hospitalizations and deaths (these can also be found in the model). From an economy perspective the ability to manage varying levels of cases without having to shut down sectors of business is critical. From the staff and teacher’s perspective how much risk will going back to work represent. For caring parents, the safety of their children is paramount. The current body of evidence suggest that the risk to children in terms of disease severity is low and that the risk of death is extremely low. [i]
Our focus in this paper is on how school reopening can impact the broad level of Covid-19 transmission (spread). Scarsin has spent hundreds of hours forecasting Covid-19 and there is a very important dynamic that is worth noting. Covid-19 is driven by an exponential virus replication process. As a result, taking the same action (like opening schools) can have very different results as you move from one health region to another and even moving along the timeline. So opening school, on Sept 8 or Sept 28 can have a much bigger impact that one might think.
Answers based on Analysis and Deep Scenario Forecasting
1. Is the risk to opening schools at the same time equal across health regions/boards?
No. the risk is not the same. Results analysis showed that health regions must be grouped into 3 risk categories. Decision support approaches for each health region risk type should be included in future scenario analysis.
The three segments of risk are:
- Minimal to no risk to reopen on schedule (Health Region 1)
- Medium risk warranting deeper scenario forecasting and a potential delay (Health Region 2)
- High risk which warrants deeper scenario forecasting and a delay to minimize risk (Health Region 3)
It is important to note that the majority of health regions have low levels of transmission and fit into the low risk category. We particularly focused our attention on larger health regions. In this case, the heath regions are over 1.2M population. Figure 1 shows three major health regions in Canada as examples of these risk groups. The graph on the left reports absolute number of reported cases along with the Stage III or Phase III reopening dates, and the graph on the right represents cases per 100,000 populations. This figure illustrates different trends and potential risks given the differences in the number of active cases within the different health regions. In this example, a TBATS statistical forecasting method was applied to forecast the future trends. The remainder of this analysis will utilize an advanced epidemiology model Scarsin has developed for forecasting and decision support, which is capable of combining agile scenarios.
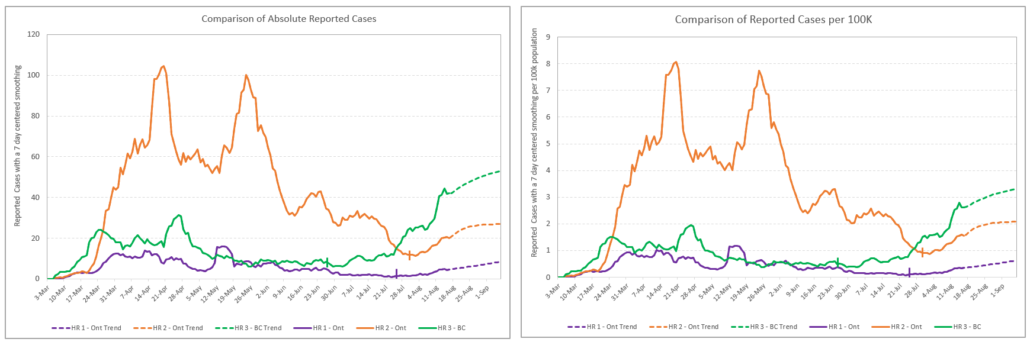
We are going to conduct a deep scenario forecasting exercise for the remainder of the paper on Health Region 2 (HR2). HR2 sits on the upper end of the medium risk assessment and could quickly change to high risk with more data points.
2. Can opening schools accelerate transmission in health regions/boards?
Yes. The degree of acceleration depends mostly on the state of the underlying transmission level and trend at the time of school opening. Inadequate decisions around school reopening timing can cause significant levels of transmission acceleration and potential unwarranted risk.
We explore this topic in layers. Figure 2 below illustrates 3 different potential trajectories that HR2 can take, given the assumption that school is opened on schedule for Sept 8. Here the red, purple and black line represent the number of cases assuming high, medium and low Covid-19 transmission level, respectively. This is meant to showcase the range of the potential risk and the uncertainty that still lies ahead.
Results show that the difference between these potential outcomes can be significant. However, the high scenario here would probably require actions in terms of a probable shut down to regain the control over disease spread. Given the high transmission rate of Covid-19, health regions will likely need to manage a level of Covid-19 above what they have experienced in full shut down (Jun-mid Aug). Shutting down the economy indefinitely bears an incredible burden to the country which also carries health and mortality risks. It is likely possible to maintain opening schools with a low wave II behavior if the testing, contact, trace and isolate capacity can maintain control.
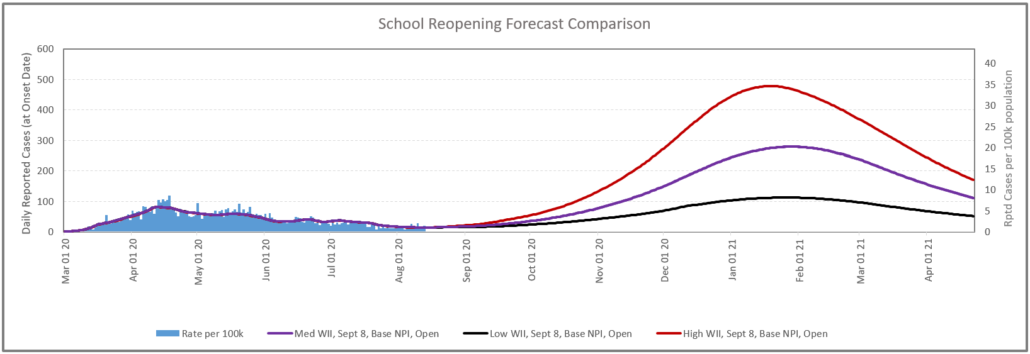
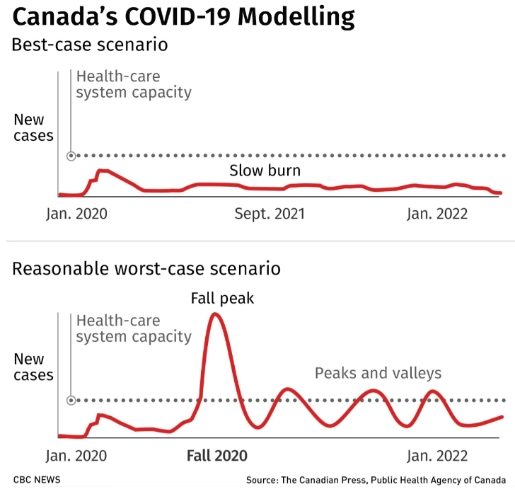
The recent PHAC update based on a new model showcases a range of potential outcomes [ii] and reinforcing the importance of Canadians staying vigilant in terms of suppression behavior. Achieving a slow burn is certainly the goal, but absorbing Stage III and opening schools add uncertainty around this outcome.
Our analysis for the school reopening did not take into consideration any additional changes in the community or workplace contact increase/decrees beyond that directly linked to the schools.
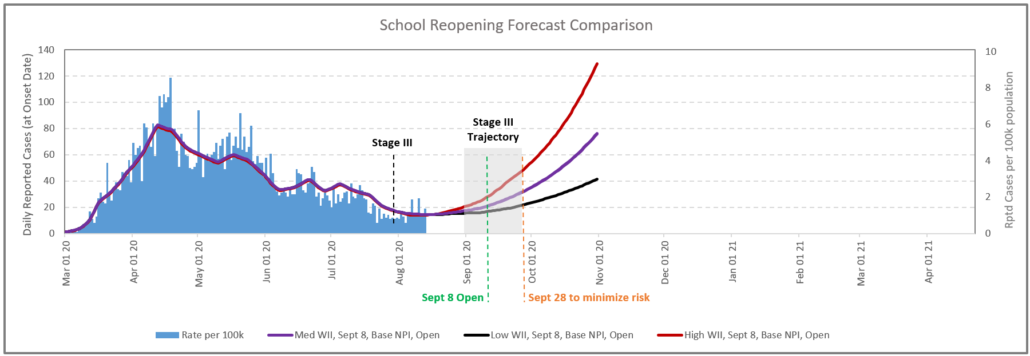
The single biggest determinant on which potential path HR2 will follow relates to post Stage III established transmission. Given the duration of the incubation period and the exponential nature of the disease transmission it seems appropriate to allow for a window of 4-6 weeks in order to observe the established disease transmission dynamics, particularly in health regions with higher population density. Our model shows that in HR2, opening school on Sept 8 provides limited insight in terms of the disease transmission dynamics. The delay in school opening to September 28 will allow for better understanding of the disease dynamic caused by Stage III opening, and therefore provides a better starting point for future decision making. For example, if within the 2 weeks the number of the cases increase above the red line, shown in Figure 3, we can conclude with high certainty that the schools should remain closed. Extending the school opening date to later date would minimize the decision risk significantly. This is a great example of how deep scenario forecasting can inform decision making.
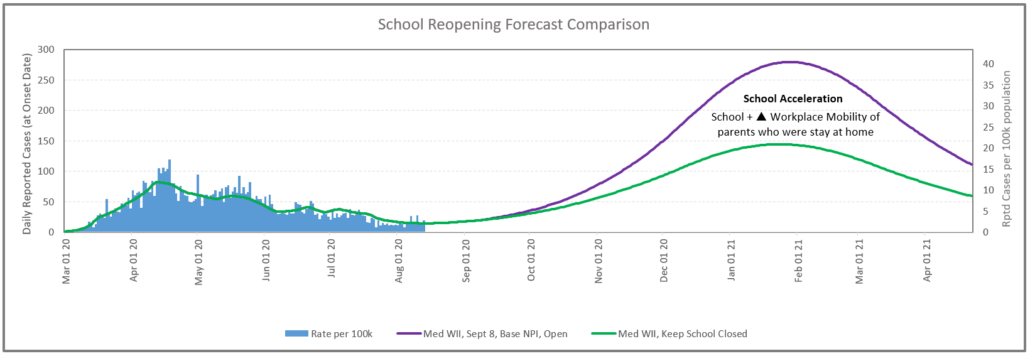
For the next layer of evaluation for HR2, we focused on the medium wave II potential outcome with a Sept 8 opening. In this case we ran a scenario (green) where we kept the school closed and compared to the scenario with school opening. The area between the curves represents the potential increase in the number of cases after the school reopening as the opening of the schools creates hundreds of thousands of new daily contacts between students, staff and teachers. School opening also has an impact on other infection locations, such as the relationship between parent mobility and child care requirements during the school year.
3a. Use of masks in younger children
Use of masks can be an effective mitigation strategy and remains a critical element of public health directives globally. Effective use of masks can have up to a 40% reduction in transmission [iii]. The key word is effective. There are limited peer reviewed studies that evaluates the sole effectiveness of masks in the 4-9 years olds in school. We utilized a lower rate of 20% efficacy for this age group and model predicted a limited impact. This however could be revisited if better reference data is made available.
Masks and respirators are commonly used to protect from respiratory infections in three different indications – for healthcare workers, sick patients and well community members [iv]. Currently there is debate and conflicting guidelines around if and how to the use of masks should be applied in school settings. CDC recommends that people wear masks in public settings and when around people who don’t live in your household, especially when other social distancing measures are difficult to maintain. Even though, the use of masks is not recommended for children under 2 years of age [v], for school aged children above 10 years of age it is highly recommended.
3b. Avoidance strategies (limiting the interactions with schools – alternating days for secondary school, opting out to online…)
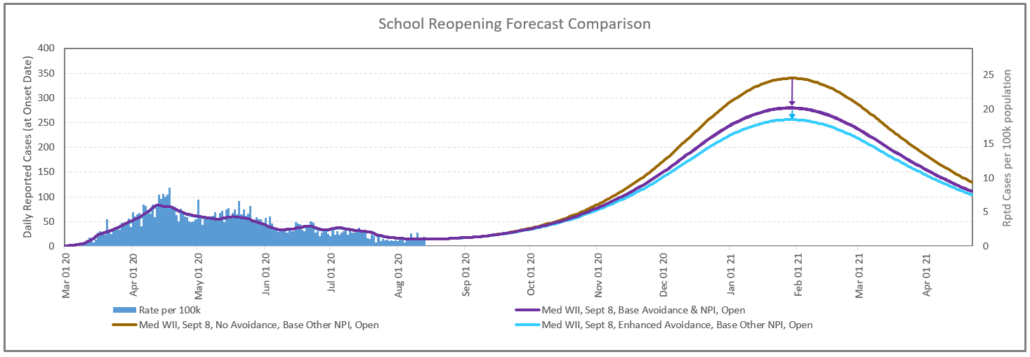
Avoidance strategies are effective in reducing the overall transmission. The secondary school alternating schedule is particularly effective. The full “opt out for online” also impacts transmission, but obviously has downside on the benefit of face to face education. Figure 5 shows the results of these forecasts based on these Table 1 assumptions.
Alternating secondary school schedule, where students attended school 2 & 3 days can result in an 11.6% reduction in contacts for the children cohort.
| Scenario | High School Schedule | Opt Out for Online |
|---|---|---|
| Med WII, Sept 8, No Avoidance, Base Other NPI, Open | No alternating schedule | No Opt out |
| Med WII, Sept 8, Base Avoidance, Base NPI, Open | 2 & 3 day alternating at secondary school | 7% increasing to 10% by Oct |
| Med WII, Sept 8, Enhanced Avoidance, Base Other NPI, Open | 2 & 3 day alternating at secondary school | 15% increasing to 20% by Oct |
3c. Other non-pharmaceutical interventions (NPIs) like social distancing, cleaning, ventilation
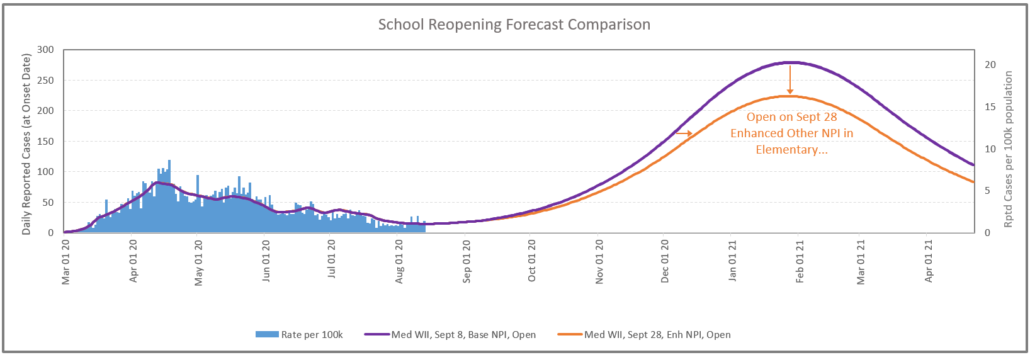
In a health region with higher density population like HR2 with medium level wave II behavior, enhanced other NPI interventions (increasing the social distancing in the classroom for elementary children along with improved ventilation and cleaning) can result in a meaningful reduction in transmission.
In order to realistically implement this, we delayed the school opening until Sept 28 in HR2. Achieving this however involves an investment in money and resources. The investment would be significant and there can be limitations, particularly when it comes to staff licensed teachers. If we were to change the focus of this question to a health region with a low population density with low levels of transmission, the enhanced measures for elementary schools would have little to no impact to the dynamic of the disease spread. This provides an example of how taking a localized approach can result in different decisions. So incurring significant expenses to implement these measures in low population density might not be a good decision or use of funds.
4. What would be the impact of an intermittent school closure policy on transmission?
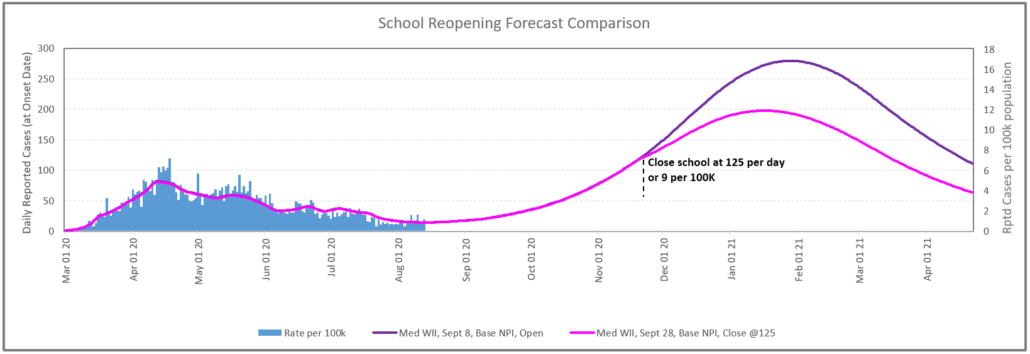
Figure 7 below provides a forecast of closing the school at 125 cases per day or 9 per 100k. This would likely represent an upper limit on the timing given the sensitivity of the community to the safety of children.
5. How important is “deep scenario forecasting” to making good decisions for schools?
Yes! It should be done at the health region level to provide the most accurate forecasts and also be able to inform local public health teams. This is ready and waiting in the Scarsin decision support system.
It is worth noting that the Scarsin decision support system can enable this type of analysis across a wide range of critical dynamics including travel (US, Intl, Domestic), vaccines, infection locations such as the home, community, workplaces by sector… This allows the system to run integrated analysis which is important as all these dynamics interplay with each other. Scarsin has gained expertise in this type of decision support working with Global 500 clients in the life sciences area across a wide array of diseases.
Limitations and Disclaimers
We have implemented methodology adjustments based on the fact that the public case data only identifies de-identified Covid-19 patients in 10 year bands. We do not believe that any of those adjustments compromise the integrity of the evaluation or answers.
This report is not meant to provide direct predictions on the de-identified health regions. It is meant to provide potential outcomes and draw insights based on varying specific parameters. It is important to note that the Scarsin solution can rerun all these scenarios as new daily data is loaded which means that even one week of additional data can change the trajectory of the forecasts either up or down.
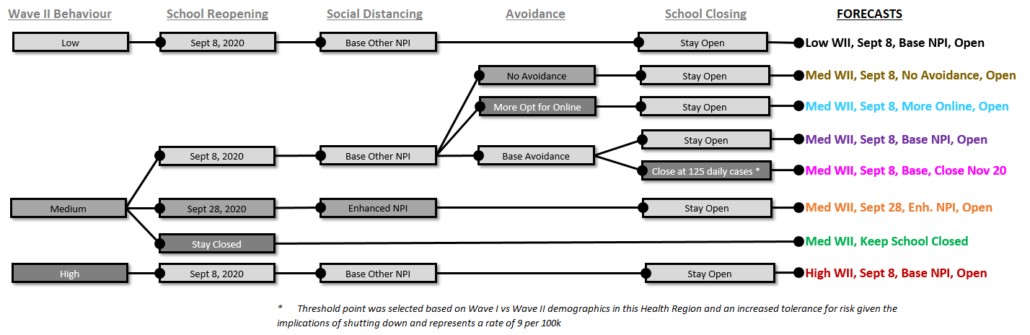
Decision Tree
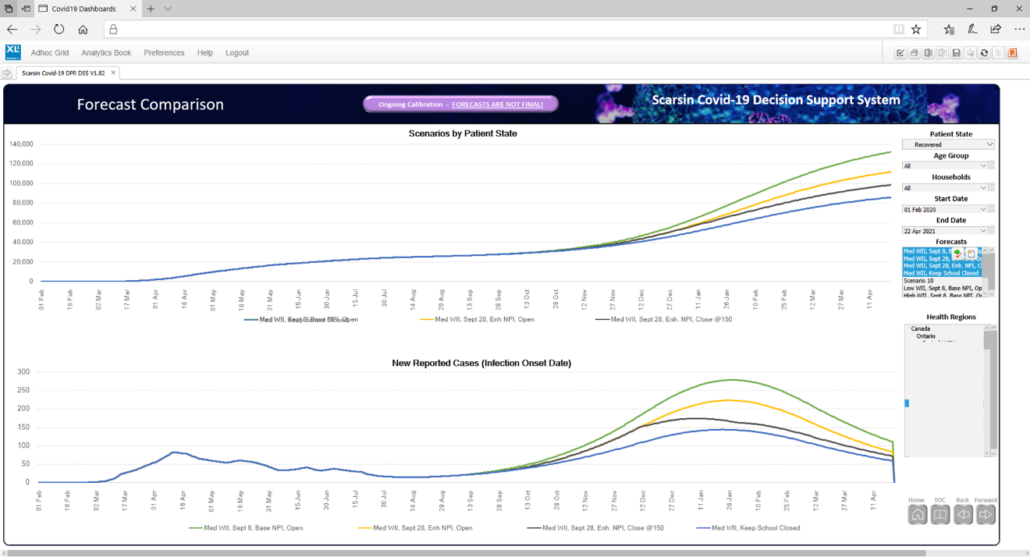
We have presented various forecasts during this report. The decision tree below showcases the different parameters that drove the forecasts presented. The colours of their names align with the colour of the lines in the graphs.
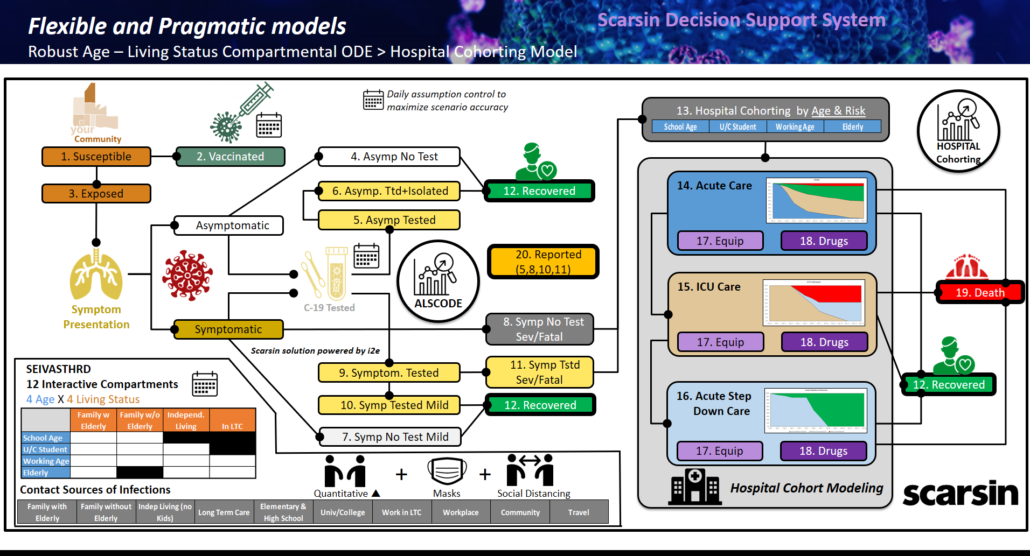
Scarsin Model Design
The figure below outlines the scenario based modeling solutions in the Scarsin platform. See “A National Crisis Deserves A National Decision Support System” in the blog section of www.scarsin-covid.com for more details.
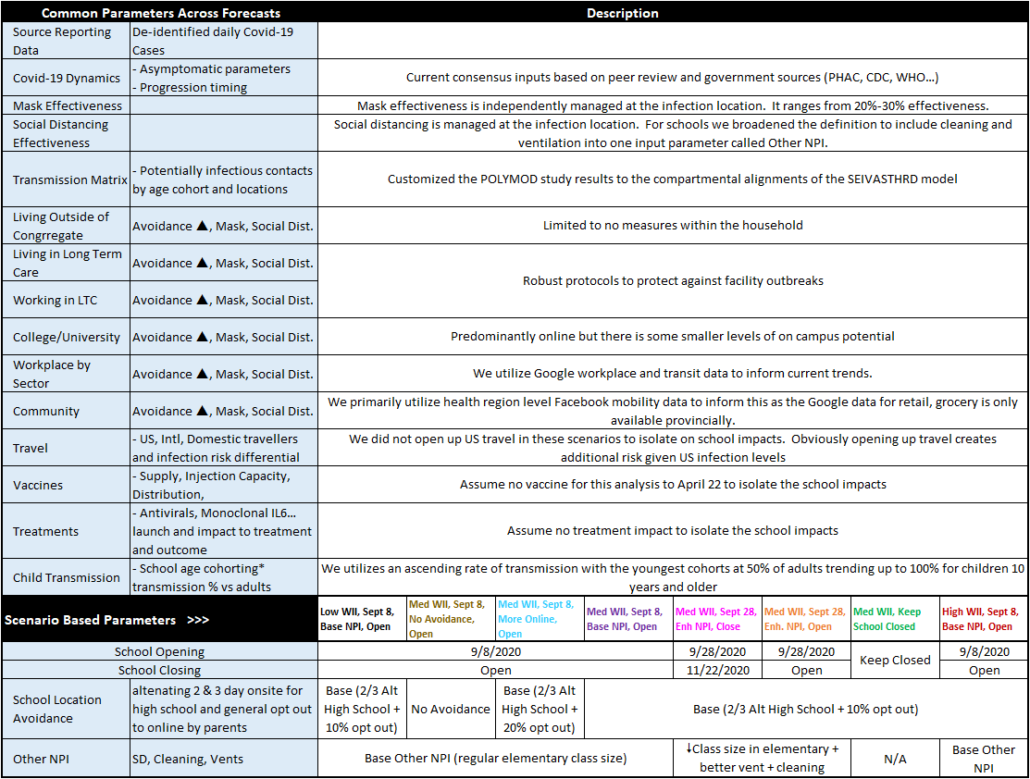
Summary of Assumption Parameters
The Scarsin ALSCODE model has >50 key areas of input. Many of those parameters enable daily event management. This table is meant to provide an overview on the broad framework we applied in this analysis.
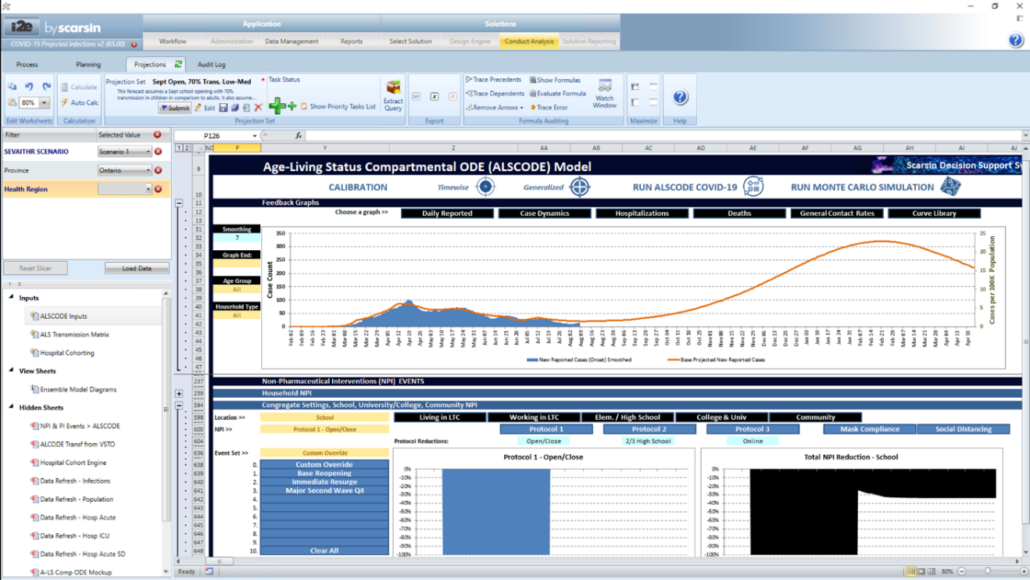
Scarsin Covid-19 Decision Support System
The screen capture below showcases the forecasting model which is enabled for all health regions in Canada. The model is undergoing constant enhancements based on its agile change management.
The screen capture below highlights the agile web dashboard for Canada
Other Information Gathered on Children & Schools
Schools create complex contact interactions.
- Busing to school, congregation behavior entering and leaving school, recess and lunch congregation, movement within the school (class rooms, hallways, bathroom…), prolonged periods within a small enclosed space (class rooms), potentially poor ventilation and air exchange
Views on child transmission
- The recent “Rapid Review: What is the specific role of daycares and schools in COVID-19 transmission?” [vi] by The National Collaborating Centre for Methods and Tools, McMaster University, August 11 version is a thorough overview of peer reviewed papers. Definitely a current review worth reading!
- CDC Update
- 7.3% of all cases of COVID-19 in the United States reported to CDC were among children (as of August 3rd, 2020) [vii]
- The number and rate of cases in children in the United States have been steadily increasing from March to July 2020
- Recent evidence suggests that children likely have the same or higher viral loads in their nasopharynx compared with adults [viii] and that children can spread the virus effectively in households and camp settings [ix,x]
- 90% increase in Child COVID-19 Cases, 7/9/20 – 8/6/20 [xi]
- Worldwide
- The emerging evidence suggests that replication of SARS-CoV-2 in older children leads to similar levels of viral nucleic acid as adults, but significantly greater amounts of viral nucleic acid are detected in children younger than 5 years [xii]
- Children over age 10 spread Covid-19 as much as adult (study by the Korea Centers for Disease Control and Prevention [xiii]
- In the case of seasonal influenza epidemics, the highest secondary attack rate occurs among young children [xiv]
The Challenges of Asymptomatic Cases
- There is strong evidence that the majority of children who get COVID-19 may not display any symptoms or have only mild symptoms (higher asymptomatic cases make testing and tracing more difficult) [xv] 66% asymptomatic in a case study in Israel [xvi]
Covid-19 with Seasonal Flu with Cold
- A major element of school procedures revolves around symptomatic presentations. These include testing and quarantining.
The challenge becomes much higher as seasonal flu and colds become prevalent. The symptom presentations are extremely overlapping. It is hopeful that Covid-19 suppression strategies reduce the normal level of seasonal flu
References/Endnotes
[i] COVID19 – What We Know So Far About…. Infection in Children https://www.publichealthontario.ca/-/media/documents/ncov/what-we-know-children-feb-21-2020.pdf?la=en
[ii] https://www.cbc.ca/news/politics/covid19-pandemic-modelling-tam-fall-peak-1.5686250
[iii] COVID-19 – What We Know So Far About…Wearing Masks in Public, Public Health Ontario June 17 update, https://www.publichealthontario.ca/-/media/documents/ncov/covid-wwksf/what-we-know-public-masks-apr-7-2020.pdf?la=en
[iv] Considerations for Wearing Masks, https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/cloth-face-cover-guidance.html
[v] A rapid systematic review of the efficacy of face masks and respirators against coronaviruses and other respiratory transmissible viruses for the community, healthcare workers and sick patients, https://www.sciencedirect.com/science/article/pii/S0020748920301139?via%3Dihub
[vi] Rapid Review: What is the specific role of daycares and schools in COVID-19 transmission, https://www.nccmt.ca/uploads/media/media/0001/02/09e652c44a7de3cfcb8d85e093cd20d8d90dc2ba.pdf
[vii] CDC. Demographic Trends of COVID-19. https://www.cdc.gov/covid-data-tracker/index.html#demographics Data retrieved July 27, 2020)
[viii] Sargent TH, Muller WJ, Zheng X, et al. Age-Related Differences in Nasopharyngeal Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Levels in Patients With Mild to Moderate Coronavirus Disease 2019 (COVID-19). JAMA Pediatrics
[ix] Park YJ, Chloe YJ, Park O, et al. Contact Tracing During Coronavirus Disease Outbreak, South Korea, 2020. Emerging Infectious Diseases
[x] Szablewski CM, Chang K, Brown MM, et al. SARS-CoV-2 transmission and infection among attendees of an overnight camp – Georgia, June. 2020. MMWR
[xii] Age-Related Differences in Nasopharyngeal Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Levels in Patients With Mild to Moderate Coronavirus Disease 2019 (COVID-19) https://jamanetwork.com/journals/jamapediatrics/fullarticle/2768952/
[xiii] Contact Tracing during Coronavirus Disease Outbreak, South Korea, 2020 https://wwwnc.cdc.gov/eid/article/26/10/20-1315_article
[xiv] Principi N, Esposito S, Marchisio P, Gasparini R, Crovari P. Socioeconomic impact of influenza on healthy children and their families. Pediatr Infect Dis J. 2003;22(Suppl):S207-10. DOIExternal LinkPubMedExternal Link
[xv] SickKids-led group of experts proposes latest guidance for school reopening https://www.sickkids.ca/AboutSickKids/Newsroom/Past-News/2020/covid19-school-guidance.html
[xvi] A large COVID-19 outbreak in a high school 10 days after schools’ reopening, Israel, May 2020, https://www.eurosurveillance.org/content/10.2807/1560-7917.ES.2020.25.29.2001352?mc_source=MTExMDY2Ojo6OTgxM2NkZDM4OGRjNGFlM2JhY2RhNWIyZTNlODhkOTE6OnYzOjoxNTk2NDc1MjIzOjox#html_fulltext
![scarsin logo black] Scarsin COVID 19](https://scarsin-covid.com/wp-content/uploads/2020/03/scarsin-logo-black.png)
